A research team led by McMaster University scientist Matthew Miller has taken one step closer to developing an effective, ‘one-punch’ flu vaccine.
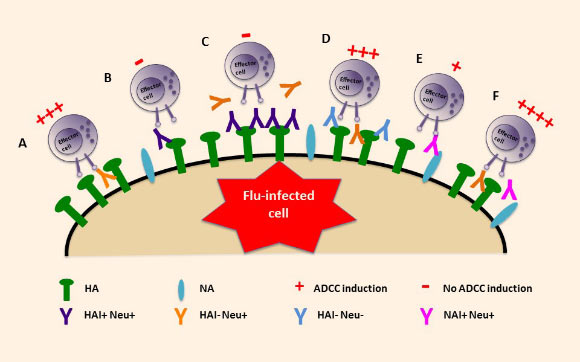
Model of ADCC (antibody-dependent cell-mediated cytotoxicity) activation by influenza A virus-specific antibody specificity. Image credit: Wenqian He et al.
While flu shots remain the best way to protect against the virus, how well a flu vaccine works each year depends on the health and age of the person being vaccinated, the similarity between seasonal vaccine viruses and circulating viruses, and whether a live or inactivated vaccine was used.
A universal flu vaccine, such as the one proposed by Dr. Miller and co-authors, could effectively prevent mismatches, since it would protect against all flu strains, and the occurrence of flu pandemics.
The team’s findings build upon their earlier discovery of a class of antibodies capable of neutralizing the most dangerous types of influenza viruses.
These antibodies essentially ‘train’ the immune system to recognize a portion of the virus that does not change from year-to-year and, in doing so, can pave the way toward a universal vaccine that needs to be given just once and could protect against all future strains of the flu, including mutated strains.
“Seasonal flu vaccines work by generating antibodies that bind to the virus and prevent it from infecting cells,” Dr. Miller said.
“Universal flu vaccines do this as well, but go one step further by recruiting white blood cells to destroy infected cells.”
Dr. Miller and his colleagues from McMaster University, the Icahn School of Medicine at Mount Sinai and the University of Chicago have discovered that while certain antibodies work well together to recruit these helpful white blood cells, others block their recruitment — and where they bind on the virus makes all the difference.
“Our findings show that just having antibodies isn’t enough,” Dr. Miller said. “You have to have antibodies that bind to very specific places on the virus.”
“Now that we know the places where antibodies have to bind, we can modify our vaccines so that we generate those antibodies in higher numbers.”
“Using this knowledge, what we can now do is specifically design our universal vaccine to generate the most desirable types of antibodies and avoid antibodies that block the functions that we want. In doing that, we can make sure that the vaccine will work in the most effective way possible,” he added.
Antibodies that recruit white blood cells are currently being studied as treatments for cancer and HIV.
The team’s results, published online today in the journal Proceedings of the National Academy of Science, are likely to improve treatments for those diseases as well.
_____
Wenqian He et al. Epitope specificity plays a critical role in regulating antibody-dependent cell-mediated cytotoxicity against influenza A virus. PNAS, published online October 3, 2016; doi: 10.1073/pnas.1609316113
This article is based on a press-release issued by McMaster University.







