A research team led by Harvard Medical School scientists has found that high levels of fructose — but not glucose — in the high-fat diet inhibit the liver’s ability to properly metabolize fat. Their results appear in the journal Cell Metabolism.
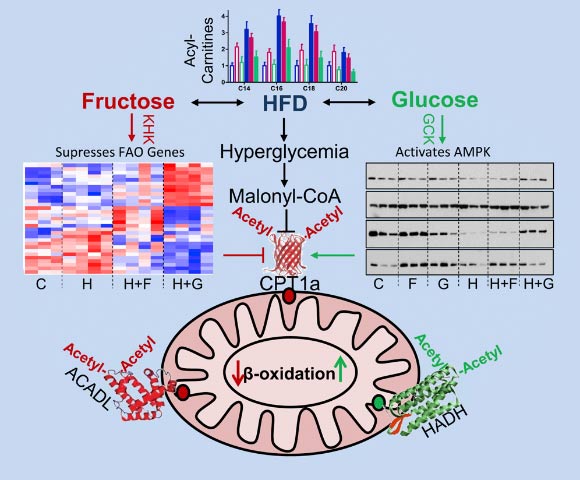
Dietary fructose, but not glucose, supplementation of high-fat diet (HFD) impairs mitochondrial size, function, and protein acetylation, resulting in decreased fatty acid oxidation and development of metabolic dysregulation. Image credit: Softic et al, doi: 10.1016/j.cmet.2019.09.003.
“Fructose makes the liver accumulate fat. It acts almost like adding more fat to the diet. This contrasts the effect of adding more glucose to the diet, which promotes the liver’s ability to burn fat, and therefore actually makes for a healthier metabolism,” said Professor C. Ronald Kahn, senior author of the study.
“The most important takeaway of this study is that high fructose in the diet is bad. It’s not bad because it’s more calories, but because it has effects on liver metabolism to make it worse at burning fat. As a result, adding fructose to the diet makes the liver store more fat, and this is bad for the liver and bad for whole body metabolism.”
“Surprisingly, when you switch the sugar in the diet from fructose to glucose, even though they’re both equally caloric, the glucose doesn’t have that effect. In fact, if anything, overall metabolism is somewhat better than if they just were on plain high-fat diet.”
“We wanted to figure out at a mechanistic level how this could be possible.”
In a series of animal studies, Professor Kahn and colleagues compared effects on metabolism of six different diets: regular chow, chow with high fructose, chow with high glucose, a high-fat diet, a high-fat diet with high fructose, and a high-fat diet with high glucose.
They analyzed different known markers of fatty liver to determine the effects of each diet. For example, they looked at levels of acylcarnitines, which are produced when the liver burns fats. High levels of these are a bad sign, since it means there is a lot of fat in the liver being burned.
Acylcarnitines were highest in the animals on the high-fat plus high fructose diet. They were lower in the high-fat plus glucose diet than in the plain high-fat diet, which reflected previous observational findings and indicated that glucose performed an assistive fat-burning action in these animals.
The team also monitored the activity of a critical enzyme for fat-burning known as CPT1a.
In the case of CPT1a, the higher the levels the better — they indicate that mitochondria are performing their fat-burning jobs correctly.
However, in the high-fat plus fructose diet, the study authors found that levels of CPT1a are low and their activity was very low, meaning mitochondria can’t function properly. This led them to investigate the mitochondria themselves.
“When mitochondria are healthy, they have this nice ovoid shape and crosshatching,” Professor Kahn said.
“In the high-fat plus fructose group, these mitochondria are fragmented and they’re not able to burn fat as well as the healthy mitochondria. But looking at the high-fat diet plus glucose group, those mitochondria become more normal looking because they are burning fat normally.”
These findings, combined with other markers they monitored, proved that both high-fat and high-fat plus fructose diets damages mitochondria and makes it easier for the liver to synthesize and store fat rather than burn it.
_____
Samir Softic et al. 2019. Dietary Sugars Alter Hepatic Fatty Acid Oxidation via Transcriptional and Post-translational Modifications of Mitochondrial Proteins. Cell Metabolism 30 (4): 735-753; doi: 10.1016/j.cmet.2019.09.003







