A study of the ‘London patient’ — the second HIV patient to undergo stem cell transplantation from donors with a HIV-resistant gene — finds that there was no active viral infection in the patient’s blood 30 months after they stopped anti-retroviral therapy; remnants of integrated HIV-1 DNA remained in his tissue samples, which were also found in the first patient to be cured of HIV, and can be regarded as so-called ‘fossils,’ as they are unlikely to be capable of reproducing the virus.
“We propose that these results represent the second ever case of a patient to be cured of HIV. Our findings show that the success of stem cell transplantation as a cure for HIV, first reported nine years ago in the Berlin patient, can be replicated,” said Professor Ravindra Kumar Gupta, a researcher at the University of Cambridge and lead author of the study.
“It is important to note that this curative treatment is high-risk, and only used as a last resort for patients with HIV who also have life-threatening hematological malignancies. Therefore, this is not a treatment that would be offered widely to patients with HIV who are on successful antiretroviral treatment.”
While most HIV patients can manage the virus with current treatment options and have the possibility of living a long and healthy life, experimental research of this kind following patients who have undergone high-risk, last-resort curative treatments, can provide insight into how a more widely applicable cure might be developed in the future.
In 2011, another patient based in Berlin — the ‘Berlin patient’ — was the first HIV patient to be reported cured of the virus 3.5 years after undergoing similar treatment.
Their treatment included total body irradiation, two rounds of stem cell transplant from a donor who carried a gene (CCR5Δ32/Δ32) that is resistant to HIV, and a chemotherapy drug regimen.
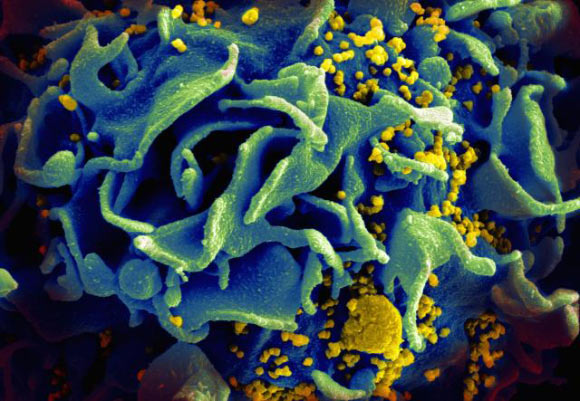
The transplant aims to make the virus unable to replicate in the patient’s body by replacing the patient’s immune cells with those of the donors, whilst the body irradiation and chemotherapy targets any residual HIV virus.
The London patient underwent one stem-cell transplantation, a reduced-intensity chemotherapy drug regimen, without whole body irradiation.
In 2019, it was reported that their HIV was in remission, and this study provides follow-up viral load blood test results at 30-months and a modeling analysis to predict the chances of viral re-emergence.
Ultrasensitive viral load sampling from the London patient’s cerebrospinal fluid, intestinal tissue, or lymphoid tissue was taken at 29 months after interruption of ART and viral load sampling of their blood at 30 months.
At 29 months, CD4 cell count (indicators of immune system health and stem cell transplantation success) was measured, and the extent to which the patient’s immune cells have been replaced by those derived from the transplant.
Results showed no active viral infection was detected in samples of the patient’s blood at 30 months, or in their cerebrospinal fluid, semen, intestinal tissue, and lymphoid tissue 29 months after stopping ART.
The patient had a healthy CD4 cell count, suggesting they have recovered well from the transplant, with their CD4 cells replaced by cells derived from the HIV-resistant transplanted stem cells.
Furthermore, 99% of the patient’s immune cells were derived from the donor’s stem cells, indicating the stem-cell transplant had been successful.
Since it was not possible to measure proportion of cells derived from the donor’s stem cells in all parts of the patient’s body (i.e. measurement was not possible in some tissue cells like lymph nodes), the scientists used a modeling analysis to predict the probability of cure based on two possible scenarios.
If 80% of patient’s cells are derived from the transplant, the probability of cure is predicted at 98%; whereas if they have 90% donor derived cells, they predict a 99% probability of cure.
“Comparing to the treatment used on the Berlin patient, the case study of the London patient represents a step towards a less intensive treatment approach, showing that the long-term remission of HIV can be achieved using reduced intensity drug regimens, with one stem cell transplant (rather than two) and without total body irradiation,” the study authors said.
“However, being only the second reported patient to undergo this experimental treatment successfully, the London patient will need continued, but much less frequent, monitoring for re-emergence of the virus.”
The team’s paper was published in The Lancet HIV.
_____
Ravindra Kumar Gupta et al. Evidence for HIV-1 cure after CCR5Δ32/Δ32 allogeneic haemopoietic stem-cell transplantation 30 months post analytical treatment interruption: a case report. The Lancet HIV, published online March 10, 2020; doi: 10.1016/S2352-3018(20)30069-2