A new inherited form of type 2 diabetes and obesity has been discovered by a team of scientists co-led by Dr Anthony Goldstone and Prof Alexandra Blakemore of Imperial College London, UK.
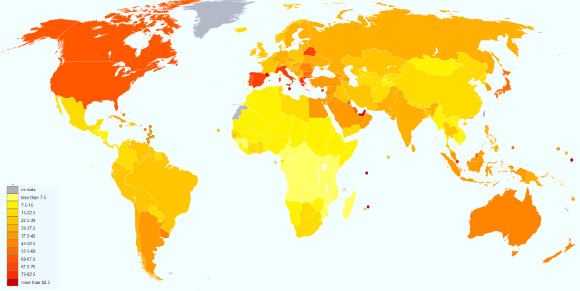
Prevalence of diabetes worldwide in 2000 (per 1,000 inhabitants). Image credit: Lokal_Profil / CC BY-SA 2.5.
A large number of genes are involved in regulating body weight, and there are now over 30 genes known in which people with harmful changes in DNA sequence become overweight. Similarly, there are a number of genes that can, when altered, cause type 2 diabetes.
These conditions are inherited through families in exactly the same way as disorders such as cystic fibrosis or Huntington’s disease.
It is unclear what proportion of severe obesity and type 2 diabetes is caused by genetic disease.
Dr Goldstone, Prof Blakemore and their colleagues discovered the new defect by sequencing the DNA of an extremely obese young woman and members of her family.
In addition to an increased appetite leading to severe weight problems from childhood, she had type 2 diabetes, learning difficulties, and reproductive problems.
The scientists found that the patient had inherited two copies of a harmful genetic change that meant she could not make carboxypeptidase-E (CPE), an enzyme that is important in the proper processing of a number of hormones and brain transmitters controlling appetite, insulin and other hormones important in the reproductive system.
Previous studies have shown that CPE deficiency causes obesity, diabetes, and impaired memory in mice, but no humans with the condition have been found before. CPE deficiency is a recessive condition, so a person would need to inherit the altered genetic sequence from both parents to be affected.
“There are now an increasing number of single-gene causes of obesity and diabetes known,” said Prof Blakemore, who is the senior author of the paper published in the journal PLoS ONE.
“We don’t know how many more have yet to be discovered, or what proportion of the severely obese people in our population have these diseases – it is not possible to tell just by looking.”
“These are serious disorders that affect the body’s ability to regulate hunger and fullness signals. They are inherited in the just same way as other genetic diseases and the sufferers should not be stigmatized for their condition. They should be offered genetic counseling and specialized lifelong support to allow them as healthy a life as possible.”
The patient was clinically evaluated; her parents are cousins, giving her a relatively high likelihood of inheriting the same genetic change from both parents. She had an older brother with similar symptoms who died aged 21.
“Finding a genetic cause for the patient’s problems has helped her and her family to understand and manage her condition better. We can also look at members of her family with one abnormal copy of the gene, to see they are affected in more subtle ways that could increase their risk of obesity,” said study first author Dr Sanne Alsters, also from Imperial College London.
“If people are diagnosed with a genetic condition like this one, we can look for other possible symptoms, and offer genetic advice to other family members if they want this. Diagnosis is very valuable to the patient. It helps to set realistic expectations, and can help them get the best possible treatment,” Prof Blakemore said.
_____
Alsters SIM et al. 2015. Truncating Homozygous Mutation of Carboxypeptidase E (CPE) in a Morbidly Obese Female with Type 2 Diabetes Mellitus, Intellectual Disability and Hypogonadotrophic Hypogonadism. PLoS ONE 10 (6): e0131417; doi: 10.1371/journal.pone.0131417







